Hematopoietic stem cell transplant saves the life of an 18-year-old with profound combined immunodeficiency.

Dr. Stuart Turvey, Dr. Henry Lu, and their colleagues at BC Children’s and UBC were surprised to find that two unrelated children from Alberta carried the same previously unknown genetic variant that leads to a dangerously weakened immune system. Experts call this profound combined immunodeficiency, or CID — a condition that can result from a wide variety of genetic and environmental causes.
The children’s immunodeficiency collectively resulted in recurring respiratory infections starting from birth, inflammatory lung disease, stunted growth, oral yeast infections, and severe colitis that required surgical removal of parts of the large intestine.
These young patients had an almost complete lack of immune protection from pathogens. Certain viruses that cause the common cold, for example, can lead to severe infection, long-term hospitalization or even death in severely immunocompromised individuals.
Working in partnership with a team of highly skilled clinicians in Alberta, Dr. Turvey, Dr. Lu and colleagues first set out to find the underlying genetic cause.
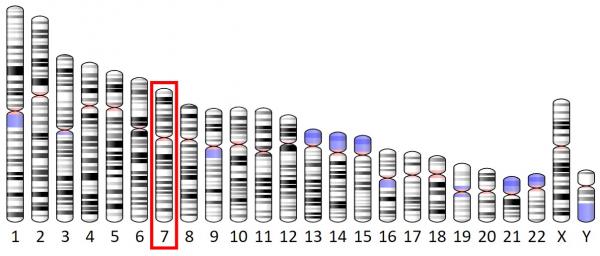
Following genetic testing, both patients were found to have a novel CARD11 gene variant that resulted in a lack of the associated protein called CARD11.
“The CARD11 protein plays an essential role in the proper development of the immune system,” said Dr. Henry Lu, a postdoctoral research fellow in the Turvey Lab at BC Children’s.
“Without this protein, we see significant abnormalities in the development and function of immune system cells called lymphocytes — specifically B cells and T cells. For example, there will be an excess of certain types of B cells and not enough of other types. We also see absent regulatory T cells, or Tregs, which control the immune system response and help prevent autoimmune disease.”

The team reported that the patients’ CID symptoms improved dramatically following hematopoietic stem cell transplantation (HSCT) performed by experts at Alberta Children’s Hospital, Calgary. HSCT is a treatment usually reserved for those with life-threatening conditions, as it presents its own set of serious complications.
“Our results support the use of HSCT in CARD11-deficient patients, and HSCT has been successfully curative in the majority of reported cases,” said Dr. Lu.
In their paper, published in The Journal of Allergy and Clinical Immunology, the researchers state the importance of diagnosing and treating CARD11 deficiency as quickly as possible.
“We look forward to continuing our work in precision health with a focus on identifying harmful genetic variants to lead to life-saving treatment for those with CARD11 deficiency,” said Dr. Lu.

The research team is co-led by Dr. Turvey and Dr. Sneha Suresh. In addition to Dr. Henry Lu, the Vancouver team includes:
- Mehul Sharma
- Dr. Christopher Overall
- Dr. Peter Bell
This research was supported by grants from the Canadian Institutes of Health Research; Genome British Columbia; the Canadian Allergy, Asthma, and Immunology Foundation; the Rare Disease Foundation; and BC Children’s Hospital Foundation.




