For more than two decades, BC Children’s Hospital researcher Dr. Megan Levings has been immersed in the complex world of very specialized immune system cells - regulatory T cells. She was the first in the world to show these unique white blood cells could be a powerful new therapy to stop harmful immune responses. Now her work has led to another giant leap forward with a first-in-the-world clinical trial in Spain involving children who are receiving heart transplants.

“We can make a significant impact in the field of transplantation,” emphasizes Dr. Levings, who is also a professor at the University of British Columbia’s Department of Surgery and School of Biomedical Engineering and the Canada Research Chair in Engineered Immune Tolerance. “When I get the opportunity to meet patients and families, I am reinvigorated to work harder and faster because I know they are counting on research to make a difference.”
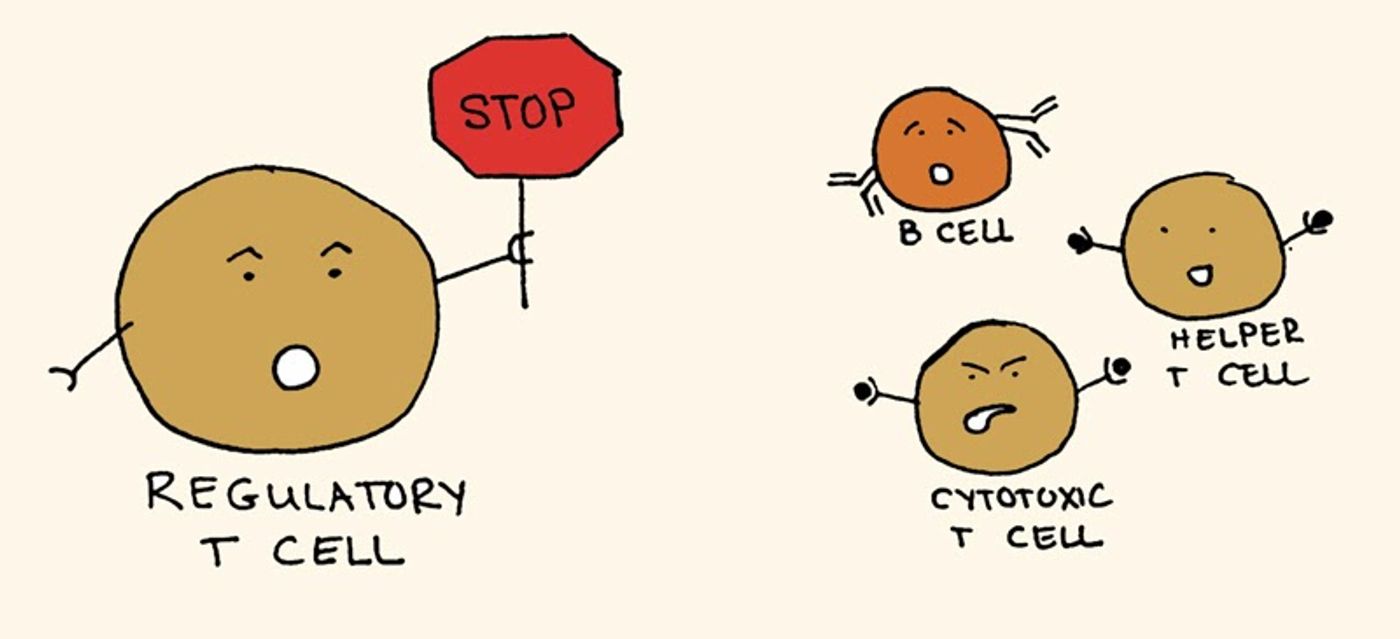
Tregs, as they are known, help orchestrate the rest of the immune system by ensuring the body doesn’t attack something it shouldn’t. Some of the first evidence for their existence was reported in 1969 and Tregs have been the subject of much study since then. Dr. Levings is internationally recognized as one of the top experts in this field of immunology and has collaborated with many other scientists around the world to keep pushing knowledge further.
Global collaborations key to new knowledge

Dr. Rafael Correa-Rocha is one of those collaborators. The pediatric immunology researcher and head of the immunoregulation laboratory at the Gregorio Marañón Health Research Institute in Madrid had also been studying the immune systems of children with heart transplants, trying to find a way to prevent rejection without the need for drugs.
Currently, transplant recipients must take drugs for the rest of their lives to suppress their immune system so it doesn't attack the donated organ. However, the drugs are toxic and come with a long list of potential side effects, including an increased chance of infections, cancer, kidney problems, diabetes and high blood pressure. Even with the medication, rejection remains a significant problem leading to high mortality in children with heart transplants. The median survival is about 15 years.
“If we can completely remove immunosuppression drugs and use Tregs to achieve immune tolerance, the state where the body tolerates the transplanted heart and doesn’t mount an immune response, then we have achieved the Holy Grail,” explains Dr. Correa-Rocha.
Finding a pediatric solution
But there was a significant roadblock to developing Treg therapy in children. In research involving adult patients, Tregs were generated from the participants’ own blood and then transfused back into the patient. This method requires 500 millilitres, or two cups of blood, which is too much to take from babies or children. There had to be another source of Tregs that would work for pediatrics. Working together, Dr. Levings and Dr. Lori West at the University of Alberta found it.
“During heart surgery on infants, thymuses are routinely removed to allow the surgeon better access to the heart. Turns out those discarded thymuses, which were just ending up in the garbage, are actually an excellent source of high-quality and potent Tregs,” says Dr. Levings. “One gram of thymus has 500 times more Tregs than one millilitre of blood.”

From the lab into humans for the first time
Dr. Correa-Rocha then developed a protocol to test the safety of infusing thymic Tregs into children who are undergoing a heart transplant. During surgery, the surgeon removes the thymus, the research team then takes the thymus and grows a large volume of Tregs, which is required for therapeutic use. The thymic Tregs are also high-quality pure cells, compared to Tregs manufactured from other sources. The expansion process takes about a week, then the cells are infused into the patient. The initial induction therapy immediately post-transplant for immune suppression has been removed, but daily medications will follow current protocol.
“These cells have never been used in a clinical trial before, especially in children,” says Dr. Correa-Rocha. “It took two years for the Spanish medical authority to approve the study. Then COVID-19 hit.”
While heart transplants didn’t halt completely during the initial wave of the pandemic, the numbers of surgeries decreased considerably. But finally in 2020, Dr. Correa-Rocha treated the first patient in the world with the thymic Treg therapy.
Spanish baby breaks new ground
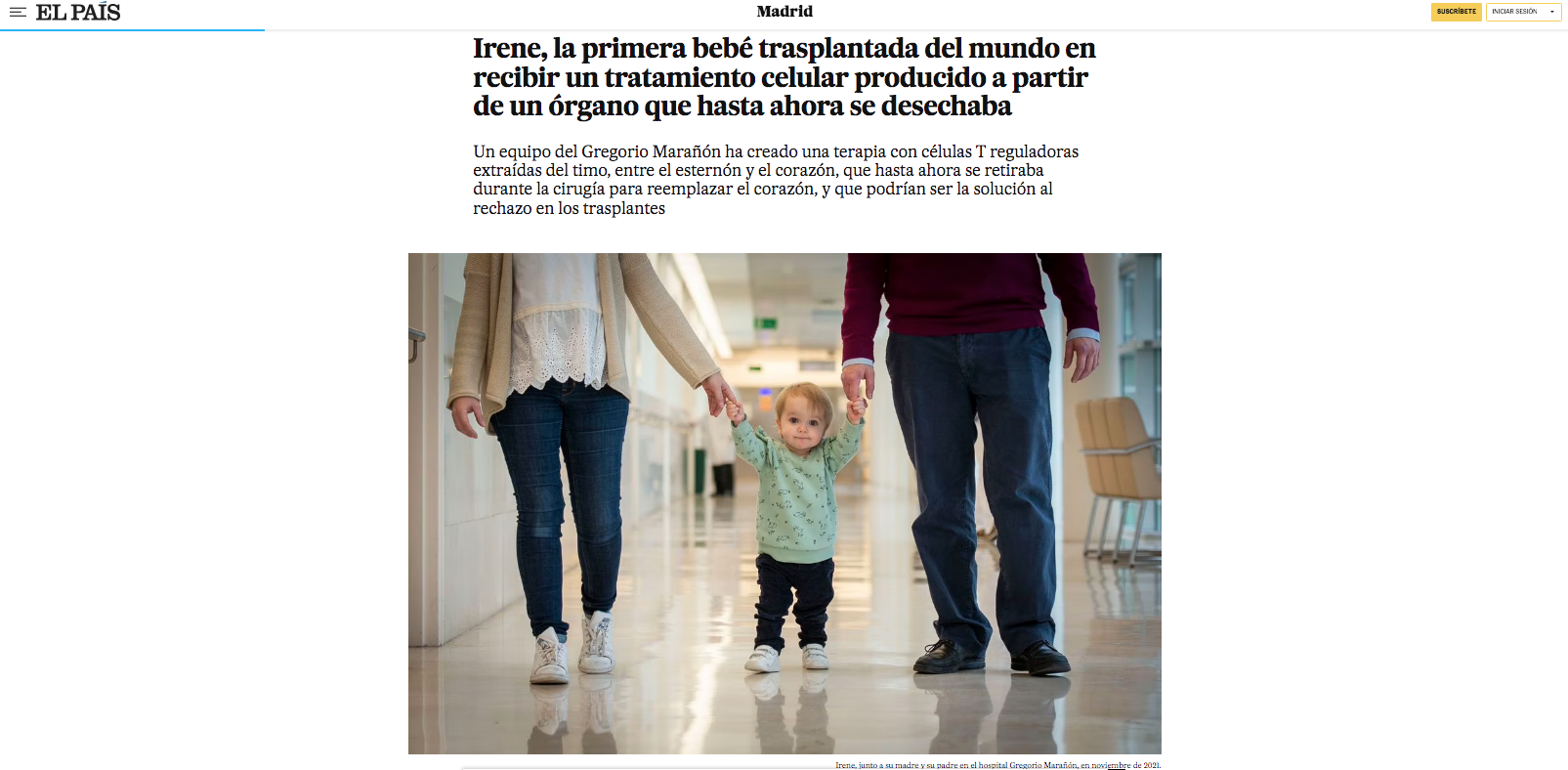
Irene was just six months old when she received a heart transplant. A week later, Treg cells expanded from her own thymus were infused into her. So far, the now three year old is doing very well.
“The results are amazing. After two years of study followup, Irene has shown no sign of rejection. And she has also maintained full levels of Treg cells following that one infusion,” says Dr. Correa-Rocha.
Compare that to pediatric heart transplant recipients who haven’t undergone the thymic Treg therapy. After two years, their Treg levels are 80 per cent lower than before transplantation. If levels can be maintained through this novel therapy, the theory is recipients wouldn’t need those toxic medications to control rejection. The Tregs would provide a natural way to police the immune system.
Opening the door to a new generation of immunotherapy
It is still early stages. Four more babies have received the thymic Treg therapy since Irene, and another three children and their families have consented to taking part in the study and are awaiting a heart transplant. If the treatment continues to prove to be safe, the next step would be to enrol these pioneers into a new clinical trial. Children who are able to maintain normal levels of Tregs would slowly reduce their immune suppression drugs. Others who have decreased levels would potentially receive another infusion of cells.

The possible uses of thymic Tregs have researchers and clinicians especially excited. For example, thymic Tregs could also be used in different individuals, children and adults, to control rejection, or treat other types of immune responses. The large volume of Tregs that can be manufactured from a single thymus would allow for hundreds of therapeutic doses.
Dr. Correa-Rocha just received approval for a study in Spain using thymic Tregs in patients hospitalized with COVID-19 who are undergoing a severe immune reaction.
Here in Canada, Dr. Levings is launching a first-in-human clinical trial of thymic Tregs to prevent graft versus host disease, a severe side effect from a bone marrow or stem cell transplant. Her lab is also working on creating the best Tregs possible with gene editing tools.
“We see the project of thymic Tregs as a platform of the future."
"These trials currently underway are setting the stage for future research with genetically modified cells,” says Dr. Levings. “And this is all using a little-known organ that is in the way of pediatric heart surgeons, and just being removed and thrown away.”
For both researchers who have spent their entire careers immersed in this field, it’s a thrilling time of hope and potential.
“It’s a dream. It’s the goal of my whole career,” enthuses Dr. Correa-Rocha.
“All my research, all the work I have done over the years is providing a benefit for patients. That’s amazing. I was always focused on immunology research that could be useful, but I never imagined it would be me personally bringing it to this stage.”




