What is Smart Discharges?
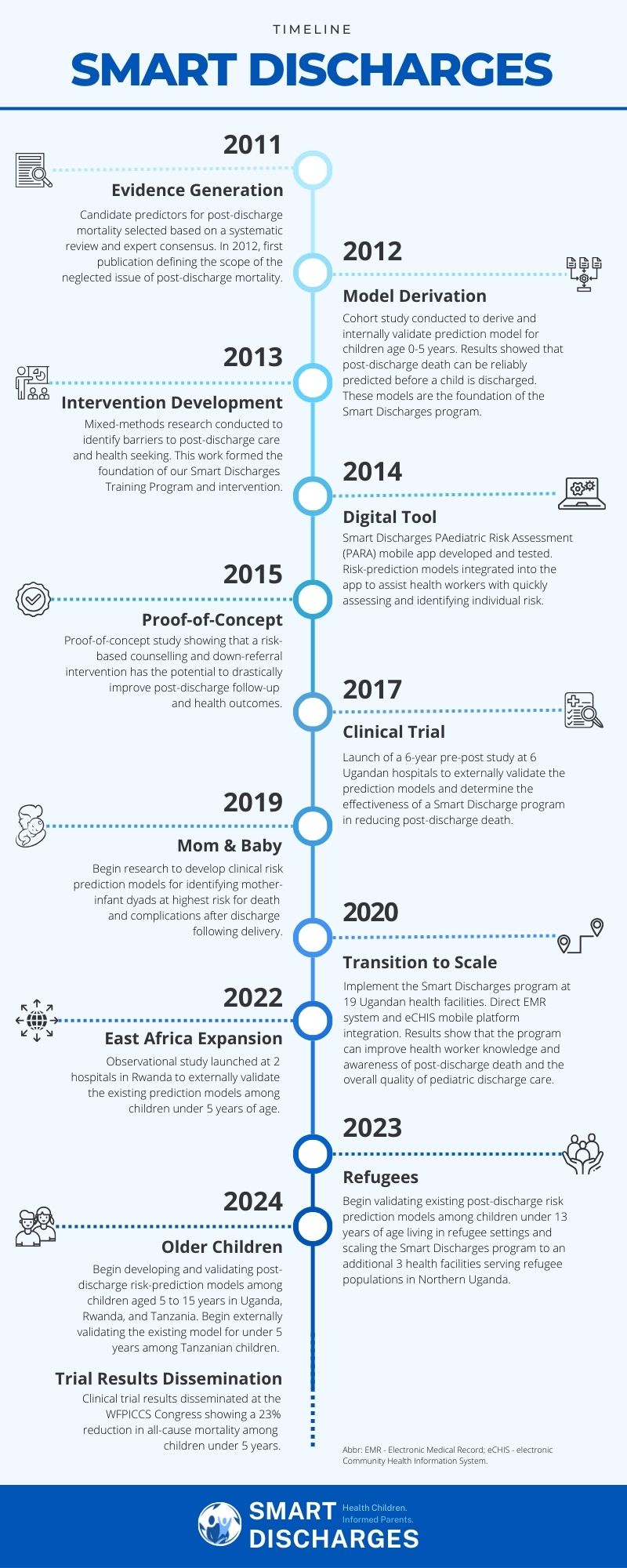
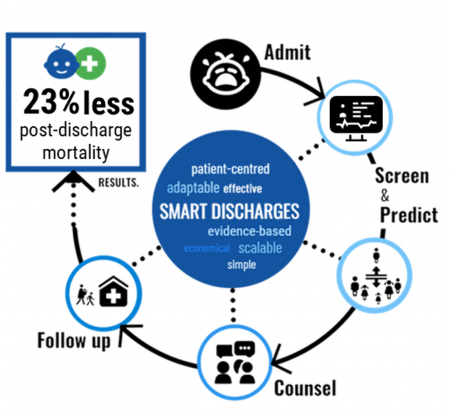 Smart Discharges is a digital health research program in East Africa that aims to improve post-discharge health outcomes in children with severe infections. By identifying at-risk children using scientifically rigorous, data-driven prediction models, health workers are able to target the delivery of personalized discharge counselling and follow-up referrals to a child’s level of risk. This is called a precision public health approach to care. Such programs can save lives and resources and are much more likely to be scalable in economically strained environments.
Smart Discharges is a digital health research program in East Africa that aims to improve post-discharge health outcomes in children with severe infections. By identifying at-risk children using scientifically rigorous, data-driven prediction models, health workers are able to target the delivery of personalized discharge counselling and follow-up referrals to a child’s level of risk. This is called a precision public health approach to care. Such programs can save lives and resources and are much more likely to be scalable in economically strained environments.
We have been working in Uganda since 2011 to better understand how to identify children at risk and to design smart interventions. Our research has shown that our risk prediction models can accurately identify children who are at high risk of dying after they leave the hospital by using up to eight routinely collected clinical and social factors collected at the time of admission. Our models are designed to work with a variety of clinical factors, allowing them to be effective even when only basic medical devices are available.
Our risk prediction models can be integrated into digital tools like diagnostic devices, electronic medical record (EMR) systems, and mobile apps to help health workers make quick, easy, and accurate decisions about discharge care. Additionally, we developed a paper-based prediction tool to ensure that health workers can use our models in any setting, even where digital resources are limited.
What is the problem?
Children hospitalized for serious infections remain vulnerable to recurring illnesses and infections even after they return home. In places like Uganda, as many children die during the first month after they are discharged from a hospital as die while in-hospital. This high rate of post-discharge mortality is observed for children treated for serious infections in countries across sub-Saharan Africa and parts of Asia.
Serious infections can include pneumonia, diarrhea, or malaria. The danger is when infections lead to sepsis. Sepsis is a life-threatening condition where the body's response to an infection damages its own tissues and organs. Sepsis is the leading cause of death from infection around the world, despite vaccines, antibiotics, and acute care. Newborn babies, children, and the elderly are especially vulnerable.
Around the world, 11 million people die of sepsis every year. A vast majority of these deaths occur in low- and middle-income countries. We believe that many of these lives can be saved by identifying vulnerable patients before they are discharged from the hospital so that we can make sure they have the tools to survive and thrive after they go home. This is the Smart Discharges approach.
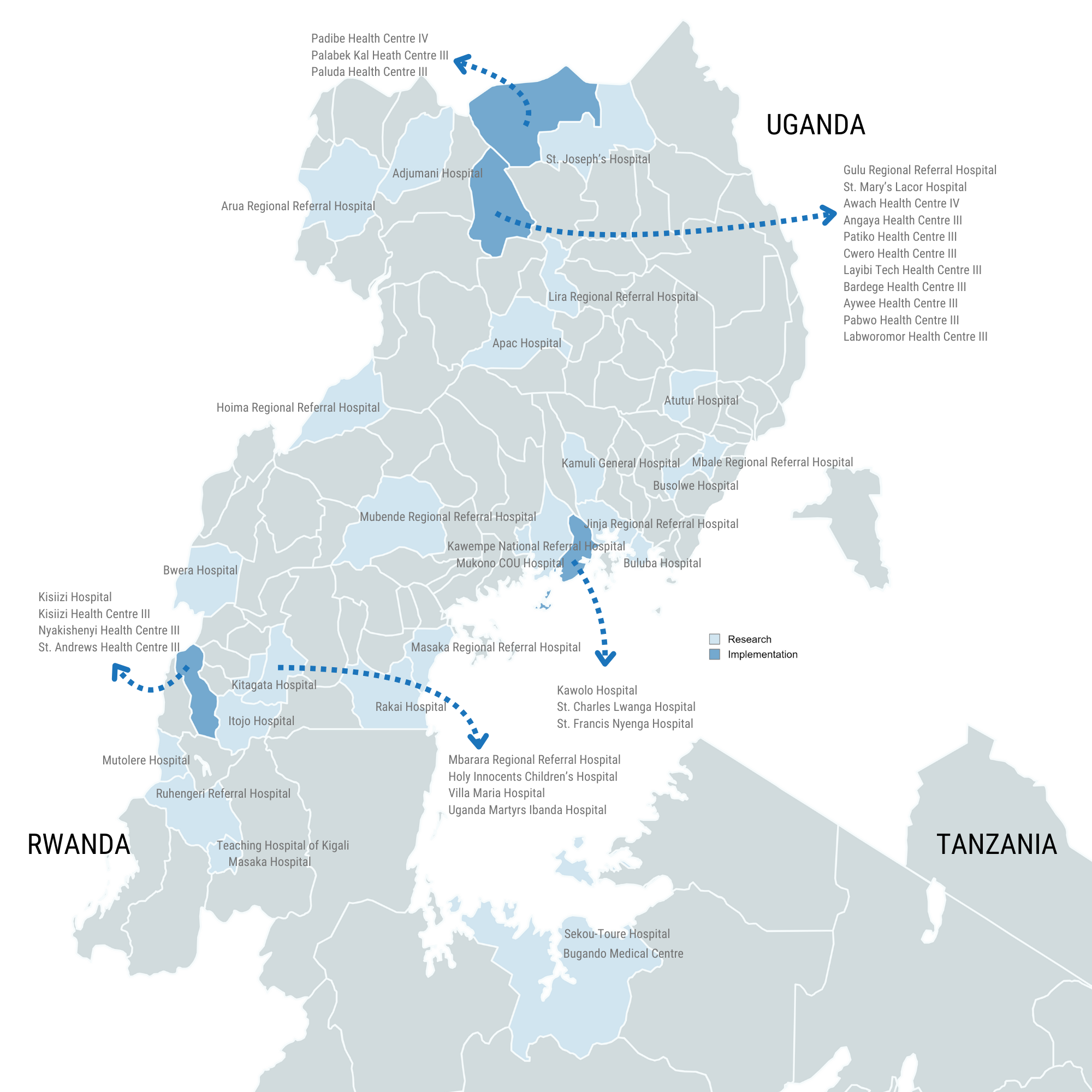
Where are Smart Discharges being used?
In partnership with the Uganda Ministry of Health, and our implementing partner, the World Alliance for Lung and Intensive Care Medicine in Uganda (WALIMU), Smart Discharges has been implemented in 22 hospitals and health centres across 4 Districts in Uganda.
Why are Smart Discharges needed?
All children who are discharged are at risk and should receive good post-discharge care. However, the resources are not always available to do this. This is why it is important to think about how to use limited resources smartly and precisely to help as many people as possible. We think about it as providing the right care to the right child at the right time. Smart Discharges help patients transition from good care in the hospital to good care in the community, with minimal changes to existing procedures. Just because a child is discharged, does not mean the illness is fully cured. Children continue to need care at home and Smart Discharges helps to ensure parents remain engaged with the health system and are equipped to ensure their child recovers well.
What is the impact?
Our recently completed clinical trial in Uganda, which included over 12,000 children and was conducted at 6 hospitals, has shown that the Smart Discharges approach reduced all-cause mortality by 23%. That means that the identification of the at-risk child and ensuring that these children receive improved care during the post-discharge period, saves lives.
The Smart Discharges + Quality Improvement (QI) intervention was implemented in 2020 at 19 health facilities across 3 districts in Uganda to determine how best to scale our innovation. Over 1,000 facility-based and community-based health workers completed the Smart Discharges Health Worker Training Program which focused on quality improvement methodology, post-discharge vulnerability, risk stratification, illness/danger sign recognition, effective peri-discharge care practices, and referrals. At 8-months post-intervention, we demonstrated that this intervention led to: i) improved and sustained discharge care processes and health worker practices; ii) improved health worker knowledge and awareness of post-discharge mortality and mitigation practices; and iii) increased discharge care satisfaction among health workers and patient-caregivers. As of 2024, the program continues to run in these facilities as part of routine care processes. We continue to make improvements to the program to ensure widespread adoption of Smart Discharges practices throughout Uganda and build capacity that ensures sustainability.
Other areas of work
Smart Discharges for Mom & Baby
In 2017, the Institute for Global Health began its work to expand the Smart Discharges program to target mother-newborn dyads. This project aims to build a clinical risk prediction model that will identify mother-infant dyads at highest risk for death and complications after discharge from hospital. Prediction of risk based on the mother and infant as a pair is a major gap in current research and vital to infant survival. In 2023, we completed an observational cohort study of post-discharge outcomes with over 7,000 mother-infant dyads admitted to two hospitals in Uganda and are now developing our initial model. Our ultimate goal is to develop an evidence-based bundle of care for both the mother and newborn, in which low-risk mother-infant pairs receive less burdensome (yet pragmatic and feasible) postpartum care, while high-risk pairs receive a more extensive bundle of interventions.
Smart Discharges for Refugees
Uganda hosts approximately 1.5 million refugees and asylum seekers, and 17% of these individuals are children under 5 years old. Both refugee and host community children in Uganda face a heightened vulnerability to severe infectious illnesses like malaria, respiratory infections, and diarrhea. However, there is a lack of epidemiological data on post-discharge mortality and morbidity for these specific sub-populations. Thus, in 2023, we launched a study at 3 health centres in Lamwo District, Northern Uganda to improve our understanding of the health outcomes and risks faced by refugee children in Uganda and validate our existing risk-prediction models among children under 13 years of age living in refugee settings.
East Africa Expansion
Between May 2022 and October 2023, we conducted an observational study among 1,000 children under 5 years admitted to 2 hospitals in Rwanda. Preliminary evidence has shown that Rwandan children suffer from very similar rates and causes of post-discharge mortality as observed in Uganda, with children under 6 months of age experiencing heightened vulnerability. Prediction models are able to accurately and reliably identify children at risk using the same key variables included in the existing under 5-year models developed in Uganda. In 2024, we will launch the same observational study among 1,000 children under 5 years admitted to 2 hospitals in Tanzania. We will use the results from this research to inform expansion of Smart Discharges across East Africa.
Smart Discharges for Older Children
Although older children have a much lower overall mortality risk than younger children, when admitted, preliminary evidence suggests that they suffer as high a risk of post-discharge death as those who are younger. In addition, sepsis can lead to persistent physical and cognitive dysfunction after hospital discharge, and data from in high-income countries demonstrates that one in three children who survive pediatric septic shock experiences a significant decline in health-related quality of life (HRQL) for at least one year following their hospitalization. However, there is no similar long-term impact of sepsis for East African children. Understanding the impact of sepsis on HRQL and functional status is required to fully characterize the burden of sepsis, and to design interventions that ensure children, and their families are able to survive and thrive.
In 2024, we launched a multi-country observational study in Uganda, Rwanda, and Tanzania to i) develop and validate post-discharge risk prediction models; ii) evaluate the health-related quality of life following severe infection; and iii) explore caregiver and health worker perceptions of discharge care. Data collection for this study will be ongoing until 2027.
Our team
The Smart Discharges team includes experts with strengths and perspectives from different fields, countries, and contexts. Walimu and the Institute for Global Health at the BC Children’s Hospital and BC Women’s Hospital and Health Centre coordinate activities for the team in tandem with their academic and implementing partners in Canada, Uganda, Rwanda, Tanzania, and the United States. Our team includes experts in child health, sepsis, neonatology, digital health, epidemiology, technology, engineering, software development, business, and program management.
Research team
- Dr. Matthew Wiens – Investigator, Institute for Global Health; Assistant Professor, UBC Department of Anesthesia, Pharmacology and Therapeutics
- Dr. Nathan Kenya-Mugisha – Executive Director, Walimu
- Dr. Niranjan “Tex” Kissoon – Professor, UBC Departments of Pediatrics and Surgery (Emergency Medicine)
- Dr. Mark Ansermino – Executive Medical Director, Global Health; Co-Director, Digital Health Innovation Lab at BC Children’s; Professor, UBC Department of Anesthesia, Pharmacology and Therapeutics
- Dr. Jerome Kabakyenga – Director, Maternal, Newborn and Child Health Institute at Mbarara University of Science and Technology
- Dr. Elias Kumbakumba – Physician/Researcher, Mbarara Regional Referral Hospital; Associate Professor, Mbarara University of Science and Technology Faculty of Medicine
- Dr. Christian Umuhoza – Physician/Researcher, University Teaching Hospital of Kigali
Software development team
- Dustin Dunsmuir – Institute for Global Health
- Phaisal Lubega – Stre@mline Health
Program management team
- Jessica Trawin – Project Manager, Institute for Global Health
- Haneen Amhaz – Project Coordinator, Institute for Global Health
- Douglas Mwesigwa – Finance & Operations Manager, WALIMU
- Clare Komugisha – Project Coordinator, WALIMU
Contact
For more information, please contact Haneen Amhaz or Matthew Wiens.
Publications
- Behan J, Kabajaasi O, Derksen B, et al. Caregivers’ and nurses’ perceptions of the Smart Discharges Program for children with sepsis in Uganda: A descriptive qualitative study. medRxiv. 2023.07.18.23292842.
- Kabajaasi O, Trawin J, Derksen B, et al. Transitions from hospital to home: A mixed methods study to evaluate pediatric discharges in Uganda. PLOS Glob Public Health. 2023. 3(9): e0002173.
- Wiens MO, Nguyen V, Bone JN, et al. Prediction models for post-discharge mortality among under-five children with suspected sepsis in Uganda: A multicohort analysis. PLOS Glob Public Health. 2024. 4(4): e0003050
- Wiens MO, Trawin J, Pillay Y, et al. Prognostic algorithms for post-discharge readmission and mortality among mother-infant dyads: an observational study protocol. Front Epidemiol. 2023;3.
- Symonds NE, Vidler M, Wiens MO, et al. Risk factors for postpartum maternal mortality and hospital readmission in low- and middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2023. 23:303;
- Knappett M, Hooft A, Maqsood MB, et al. Verbal Autopsy to Assess Postdischarge Mortality in Children With Suspected Sepsis in Uganda. Pediatrics. 2023;152(5):e2023062011.
- Wiens MO, Bone JN, Kumbakumba E, et al. Mortality after hospital discharge among children younger than 5 years admitted with suspected sepsis in Uganda: a prospective, multisite, observational cohort study. Lancet Child Adolescent Health. 2023
- Akech SK, T.; Wiens, M.O.; Chandna, A.; Berkley, J.A.; Snow, R.W. Tackling post-discharge mortality in children living in LMICs to reduce child deaths. Lancet Child and Adolescent Health. 2023;
- Wiens MO, Kissoon N, Holsti L. Challenges in pediatric post-sepsis care in resource limited settings: a narrative review. Transl Pediatr 2021; 10(10): 2666-77.
- Krepiakevich A, Khowaja AR, Kabajaasi O, et al. Out of pocket costs and time/productivity losses for pediatric sepsis in Uganda: a mixed-methods study. BMC Health Serv Res. 2021; 21(1): 1252.
- Nemetchek B, Khowaja A, Kavuma A, et al. Exploring healthcare providers' perspectives of the paediatric discharge process in Uganda: a qualitative exploratory study. BMJ Open. 2019; 9(9): e029526.
- Wiens MO, Kissoon N, Kabakyenga J. Smart Hospital Discharges to Address a Neglected Epidemic in Sepsis in Low- and Middle-Income Countries. JAMA Pediatrics. 2018; 172(3): 213-4.
- Nemetchek BR, Liang LD, Kissoon N, et al. Predictor variables for post-discharge mortality modelling in infants: a protocol development project. African Health Sciences. 2018; 18(4): 1214-25.
- Nemetchek B, English L, Kissoon N, et al. Paediatric postdischarge mortality in developing countries: a systematic review. BMJ Open. 2018; 8(12): e023445.
- Liang LD, Kotadia N, English L, et al. Predictors of Mortality in Neonates and Infants Hospitalized With Sepsis or Serious Infections in Developing Countries: A Systematic Review. Frontiers in Pediatrics. 2018; 6: 277.
- Wiens MO, Larson CP, Kumbakumba E, et al. Application of Sepsis Definitions to Pediatric Patients Admitted With Suspected Infections in Uganda. Pediatric Critical Care Medicine. 2016; 17(5): 400-5.
- Wiens MO, Kumbakumba E, Larson CP, et al. Scheduled Follow-Up Referrals and Simple Prevention Kits Including Counseling to Improve Post-Discharge Outcomes Among Children in Uganda: A Proof-of-Concept Study. Global Health, Science and Practice. 2016; 4(3): 422-34.
- Wiens MO, Kissoon N, Kumbakumba E, et al. Selecting candidate predictor variables for the modelling of post-discharge mortality from sepsis: a protocol development project. African Health Sciences. 2016; 16(1): 162-9.
- Lowlaavar N, Larson CP, Kumbakumba E, et al. Pediatric in-Hospital Death from Infectious Disease in Uganda: Derivation of Clinical Prediction Models. PloS One. 2016; 11(3): e0150683.
- English L, Kumbakumba E, Larson CP, et al. Pediatric out-of-hospital deaths following hospital discharge: a mixed-methods study. African Health Sciences. 2016; 16(4): 883-91.
- English LL, Dunsmuir D, Kumbakumba E, et al. The PAediatric Risk Assessment (PARA) Mobile App to Reduce Postdischarge Child Mortality: Design, Usability, and Feasibility for Health Care Workers in Uganda. JMIR mHealth and uHealth. 2016; 4(1): e16.
- Wiens MO, Kumbakumba E, Larson CP, et al. Postdischarge mortality in children with acute infectious diseases: derivation of postdischarge mortality prediction models. BMJ Open. 2015; 5(11): e009449.
- Wiens MO, Gan H, Barigye C, et al. A cohort study of morbidity, mortality and health seeking behavior following rural health center visits by children under 12 in southwestern Uganda. PloS One. 2015; 10(1): e0118055.
- Wiens MO, Pawluk S, Kissoon N, et al. Pediatric post-discharge mortality in resource poor countries: a systematic review. PloS One. 2013; 8(6): e66698.
- Wiens MO, Kumbakumba E, Kissoon N, Ansermino JM, Ndamira A, Larson CP. Pediatric sepsis in the developing world: challenges in defining sepsis and issues in post-discharge mortality. Clinical Epidemiology. 2012; 4: 319-25.
Support and thanks
The Smart Discharges team gratefully acknowledges our partners and funders. Better discharge care is a team effort, and we wouldn’t be able to do this work without the dedication and support of all those involved in making this program a reality.
Partners

Funders